Medicalbillingclaim denials can significantly impact a healthcare provider’s revenue cycle management. Did you know that nearly 30% of claims are denied on the first submission? This blog post will explore key factors leading to these denials, including incomplete patient information, coding errors, and issues with prior authorization. By understanding these common pitfalls, healthcare providers can improve their claims processing and enhance their denial management strategies. This content will help identify specific problems in the medicalbilling process, ultimately leading to better insurance verification and increased revenue.
Incomplete or Incorrect Patient Information
Incomplete or incorrect patient information is a significant factor contributing to medicalbillingclaim denials. Common mistakes in recording patient details can lead to invalid insurance information, affecting claims processing. Verifying patient data, including copayment and Medicare details, is essential to prevent these denials and ensure accurate electronic health record management in health care settings.
Common Mistakes in Recording Patient Details
Common mistakes in recording patient details can significantly impact medicalbilling and reimbursement processes. Errors such as incorrect insurance information or missing copayment details can lead to claim denials, forcing healthcare providers to appeal for payment. Under the Affordable Care Act, accurate patient information is crucial for ensuring that claims related to various diseases are processed efficiently, ultimately affecting the financial health of medical practices.
Impact of Invalid Insurance Information on Claims
Invalid insurance information can lead to significant claim denials, impacting the financial stability of healthcare providers. When a medical record contains errors related to the insurer or Medicaid details, it creates a failure in the claims process, resulting in delayed payments or outright denials. To mitigate these issues, healthcare practices must prioritize accurate data entry and verification, ensuring that all patient information is correct before submitting claims to insurers.
Verifying Patient Data to Prevent Denials
Verifying patient data is a critical step in preventing claim denials during the adjudication process. Accurate information regarding health insurance, including primary care details and copayment fees, ensures that claims for services such as physical therapy are processed smoothly. By implementing thorough verification procedures, healthcare providers can significantly reduce the risk of errors that lead to financial setbacks and enhance their overall billing efficiency.
Coding Errors and Mismatches
Coding Errors and Mismatches
Coding errors and mismatches are a primary reason for medicalbillingclaim denials. Inaccurate medical codes can lead to rejected claims, affecting reimbursement for services such as therapy. Ensuring the correct use of ICD and CPT codes is essential, along with staying updated on coding guidelines set by the American National Standards Institute. These practices help maintain compliance with policy requirements and improve claims processing efficiency.
Consequences of Inaccurate Medical Codes
Inaccurate medical codes can severely disrupt the workflow of healthcare providers, leading to claim denials and delayed reimbursements. For instance, when a patient receives mental health services, incorrect coding may result in the denial of claims by preferred provider organizations, complicating the billing process. Additionally, discrepancies in coding can lead to confusion in remittance advice, making it challenging for providers to understand payment issues and rectify them promptly.
Ensuring Correct Use of ICD and CPT Codes
Ensuring the correct use of ICD and CPT codes is vital for effective medicalbilling and reducing claim denials. Organizations must conduct regular audits to verify that coding aligns with the medical necessity of the services provided by physicians. By implementing comprehensive training programs for coding staff and utilizing updated coding resources, healthcare providers can enhance accuracy and compliance, ultimately improving their reimbursement rates and minimizing financial losses.
Regular Updates on Coding Guidelines
Regular updates on coding guidelines are essential for minimizing denied claims in medicalbilling. Healthcare providers must stay informed about changes in regulations and contract requirements to ensure compliance and accuracy in coding practices. For instance, timely updates can help prevent discrepancies in remittance advice, which often arise from outdated codes, ultimately leading to smoother claims processing and improved reimbursement rates.
Lack of Prior Authorization
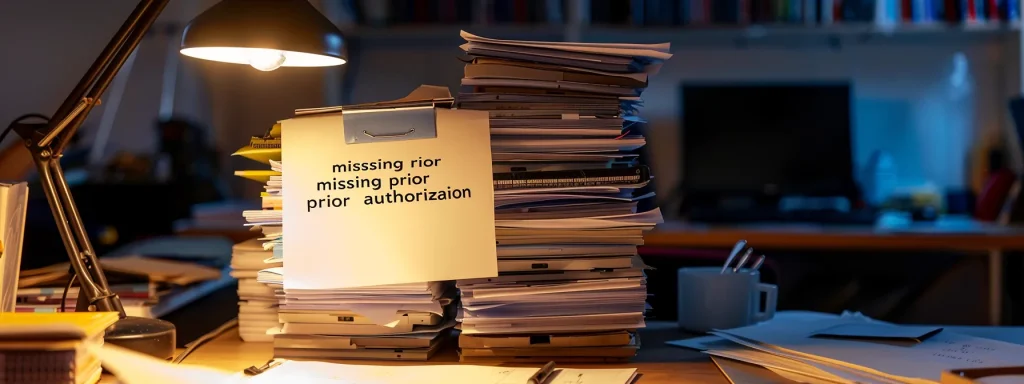
Lack of Prior Authorization
Lack of prior authorization is a critical factor contributing to medicalbillingclaim denials. Identifying procedures that require pre-approval is essential for ensuring compliance and securing revenue. Streamlining the authorization process can help healthcare providers avoid delays, while effectively handling denials due to missing authorizations is vital for managing medication and drug-related claims. Each of these aspects plays a significant role in enhancing billing efficiency and minimizing financial losses.
Identifying Procedures That Require Pre-Approval
Identifying procedures that require pre-approval is essential for healthcare providers to avoid claim denials related to lack of prior authorization. Many insurance plans mandate pre-authorization for specific services, such as surgeries or advanced imaging, to ensure medical necessity. By implementing a systematic approach to verify which procedures need pre-approval, providers can streamline the authorization process, reduce delays, and enhance their overall billing efficiency.
Streamlining the Authorization Process
Streamlining the authorization process is essential for healthcare providers to minimize claim denials due to lack of prior authorization. By implementing efficient workflows and utilizing technology, such as automated systems for tracking authorization requests, providers can ensure timely approvals for necessary procedures. This proactive approach not only enhances billing efficiency but also improves patient care by reducing delays in treatment, ultimately safeguarding the financial health of medical practices.
Handling Denials Due to Missing Authorizations
Handling denials due to missing authorizations requires a systematic approach to ensure timely resolution and minimize financial losses. Healthcare providers should establish a dedicated team to review denied claims, identify the reasons for the lack of prior authorization, and communicate effectively with insurance companies to appeal these denials. By implementing a robust tracking system for authorization requests, providers can enhance their billing processes and reduce the likelihood of future denials, ultimately safeguarding their revenue cycle.
Insurance Coverage Issues

Insurance Coverage Issues
Insurance coverage issues play a crucial role in medicalbillingclaim denials. Understanding policy limitations and exclusions is essential for healthcare providers to navigate the complexities of insurance plans. Verifying patient eligibility and benefits ensures that services are covered, while managing claims for non-covered services helps mitigate financial losses. Each of these aspects is vital for effective billing practices.
Understanding Policy Limitations and Exclusions
Understanding policy limitations and exclusions is essential for healthcare providers to effectively manage medicalbilling and avoid claim denials. Many insurance plans have specific criteria that dictate what services are covered, and failing to recognize these limitations can lead to unexpected financial burdens for both providers and patients. By thoroughly reviewing insurance policies and confirming patient eligibility before providing services, healthcare practices can minimize the risk of denied claims and ensure that they receive appropriate reimbursement for the care they deliver.
Verifying Patient Eligibility and Benefits
Verifying patient eligibility and benefits is a critical step in the medicalbilling process that can significantly reduce claim denials. Healthcare providers must confirm that patients have active insurance coverage and understand the specifics of their benefits before delivering services. This proactive approach not only ensures that the services rendered are covered but also helps avoid unexpected financial burdens for both the provider and the patient, ultimately enhancing the efficiency of the billing process.
Managing Claims for Non-Covered Services
Managing claims for non-covered services is a critical aspect of medicalbilling that requires careful attention to detail. Healthcare providers must clearly communicate with patients about their insurance coverage limitations before delivering services. By proactively discussing potential out-of-pocket costs and documenting these conversations, providers can minimize disputes and ensure that patients are aware of their financial responsibilities, ultimately reducing the risk of claim denials related to non-covered services.
Late Submission of Claims

Late Submission of Claims
Adhering to payer submission deadlines is crucial in the medicalbilling process. Implementing efficient billing practices can help healthcare providers avoid the consequences of delayed claim filing, which often leads to claim denials. This section will explore the importance of timely submissions, strategies for improving billing efficiency, and the financial impact of late claims on healthcare practices.
Adhering to Payer Submission Deadlines
Adhering to payer submission deadlines is essential for healthcare providers to avoid claim denials related to late submissions. Each insurance company has specific timelines for when claims must be filed, and missing these deadlines can result in automatic denials, impacting the financial health of medical practices. By implementing efficient billing workflows and utilizing technology to track submission dates, providers can ensure timely filing and maintain a steady revenue stream.
Implementing Efficient Billing Practices
Implementing efficient billing practices is essential for healthcare providers to minimize late submission of claims, which can lead to denials. By utilizing automated billing systems, practices can streamline their workflows, ensuring that claims are submitted promptly and accurately. Regular training for billing staff on submission deadlines and payer requirements further enhances compliance, ultimately safeguarding the financial health of medical practices.
Consequences of Delayed Claim Filing
Delayed claim filing can have significant financial repercussions for healthcare providers. When claims are submitted late, they often face automatic denials from insurance companies, which can disrupt cash flow and lead to increased administrative costs associated with appeals. To mitigate these consequences, healthcare practices must prioritize timely submissions and implement efficient billing workflows that ensure claims are filed within the required deadlines.
Missing or Incomplete Documentation
Missing or Incomplete Documentation
Comprehensive medical records are essential for successful medicalbilling and reducing claim denials. Gathering necessary supporting documents ensures that all required information is available for claims processing. Additionally, auditing documentation before submission helps identify gaps and inaccuracies, ultimately enhancing the accuracy of claims and improving reimbursement rates.
Importance of Comprehensive Medical Records
Comprehensive medical records are vital for successful medicalbilling and minimizing claim denials. Accurate and complete documentation provides the necessary support for claims, ensuring that all required information is available for processing. For instance, when healthcare providers maintain thorough records of patient visits, treatments, and diagnoses, they significantly enhance their chances of receiving timely reimbursements and reduce the likelihood of disputes with insurance companies.
Gathering Necessary Supporting Documents
Gathering necessary supporting documents is crucial for successful medicalbilling and minimizing claim denials. Healthcare providers must ensure that all relevant documentation, such as patient records, treatment notes, and referral letters, is complete and accurate before submitting claims. By implementing a systematic approach to collect and verify these documents, providers can significantly enhance their chances of receiving timely reimbursements and reduce the risk of disputes with insurance companies.
Auditing Documentation Before Submission
Auditing documentation before submission is a critical step in the medicalbilling process that can significantly reduce claim denials. By thoroughly reviewing patient records, treatment notes, and referral letters, healthcare providers can identify any gaps or inaccuracies that may lead to issues during claims processing. Implementing a systematic auditing process not only enhances the accuracy of submitted claims but also ensures compliance with insurance requirements, ultimately improving reimbursement rates and safeguarding the financial health of medical practices.
Key Strategies to Prevent Medical Billing Claim Denials
Understanding the key factors leading to medicalbillingclaim denials is crucial for healthcare providers aiming to maintain financial stability. Inaccurate patient information, coding errors, lack of prior authorization, and insurance coverage issues can significantly disrupt the billing process and delay reimbursements. By prioritizing accurate data entry, regular audits, and effective communication with patients and insurers, providers can minimize the risk of denials. Implementing these strategies not only enhances billing efficiency but also safeguards the overall financial health of medical practices.
Visit our services for more details.
Visit our homepage for more details. easycarebilling.com. Contact us Today @ 502-514-9155
Instagram: https://www.instagram.com/medicalbillling/
Twitter: https://twitter.com/vicky_easycare
Frequently Asked Questions
What is revenue cycle management in healthcare?
Revenue cycle management in healthcare is the financial process of handling medical billing, from patient registration to final payment, ensuring efficient revenue flow and compliance.
What are the critical components for revenue cycle success?
Critical components for revenue cycle success in medical billing include accurate patient registration, timely claim submission, effective denial management, and robust payment processing.
How does patient registration affect healthcare revenue?
Patient registration initiates the healthcare revenue cycle, ensuring accurate patient information for billing and reducing claim denials, directly impacting revenue efficiency and the financial health of medical practices.
Why is accurate medical coding essential in billing?
Accurate medical coding is crucial for ensuring proper billing, maximizing reimbursement, and avoiding costly errors or claim denials in healthcare management.
What strategies enhance revenue cycle efficiency in healthcare?
Optimizing revenue cycle efficiency in healthcare hinges on integrating electronic health records, automating billing processes, and training staff in effective claims management.


